For most people, a bad night of sleep means fatigue and irritability the next day.
For someone with bipolar disorder, it can mean something much bigger: the beginning of a mood episode.
Sleep is not just a wellness add-on in bipolar disorder. It is a central regulator of mood stability, biologically, psychologically, and behaviorally. When sleep becomes irregular, bipolar symptoms often follow. That’s why protecting sleep isn’t optional.
Sleep and Bipolar Disorder: Why Protecting Your Sleep Is Non-Negotiable
Bipolar Disorder Is a Circadian Rhythm Condition
At its core, bipolar disorder is closely tied to disruptions in circadian rhythm which is the body’s internal 24-hour clock, coordinated by the suprachiasmatic nucleus in the hypothalamus. This clock regulates:
Melatonin release
Cortisol patterns
Core body temperature
Alertness and energy
Sleep–wake timing
Research consistently shows that people with bipolar disorder have greater circadian sensitivity and instability compared to the general population. Even small disruptions like staying up late, traveling across time zones, pulling an all-nighter can destabilize mood.
In fact, reduced need for sleep is often one of the earliest warning signs of mania or hypomania. Sometimes it’s the first symptom.
Sleep Loss Doesn’t Just Reflect Mania, It Can Trigger It
Many patients describe the same pattern:
“I stayed up late one night, felt fine the next day… then energized… then wired… and suddenly I wasn’t sleeping at all.”
Experimental sleep deprivation studies show that even one night of reduced sleep can induce hypomanic or manic symptoms in vulnerable individuals. The mechanism likely involves:
Increased dopaminergic activity
Altered reward sensitivity
Disruption of emotional regulation circuits
HPA-axis activation
Sleep deprivation temporarily increases dopamine signaling, which may explain why some people initially feel productive or euphoric. But the crash often follows.
Depression Has a Sleep Signature Too
While mania is linked to decreased need for sleep, bipolar depression often brings:
Hypersomnia
Fragmented sleep
Delayed sleep phase (very late bedtime/wake time)
Early morning awakening
Non-restorative sleep
This irregularity can perpetuate depressive episodes through inflammatory signaling, circadian misalignment, and impaired emotional regulation.
The key point: both poles of bipolar disorder involve disrupted sleep architecture.
Why “Catching Up on Sleep” Doesn’t Work
Many people try to compensate after poor sleep by:
Sleeping in excessively
Napping unpredictably
Shifting bedtime dramatically
Unfortunately, this often worsens circadian instability. The brain thrives on regularity. In bipolar disorder, consistency matters more than duration alone.
Protecting sleep means stabilizing the rhythm.
The Sleep–Light Connection
Light is the most powerful circadian regulator. Evening light exposure, especially blue light from screens, suppresses melatonin and delays sleep onset.
In bipolar disorder, the brain may be particularly sensitive to light shifts. Research suggests that:
Late-night light exposure can trigger mood elevation in some individuals
Morning bright light (used carefully) can help bipolar depression when monitored properly
Seasonal light variation influences mood in vulnerable patients
This is why structured light exposure and dark-time protection can be helpful.
Therapy Models Built Around Sleep Stability
Interpersonal and Social Rhythm Therapy (IPSRT), an evidence-based treatment for bipolar disorder, centers on one principle: stabilize daily rhythms to stabilize mood.
IPSRT focuses on:
Consistent wake time (even on weekends)
Regular mealtimes
Structured daily activity
Predictable bedtime
Monitoring early warning signs
Medication management and therapy are most effective when sleep is stable. Without rhythm stability, even well-designed medication regimens can struggle.
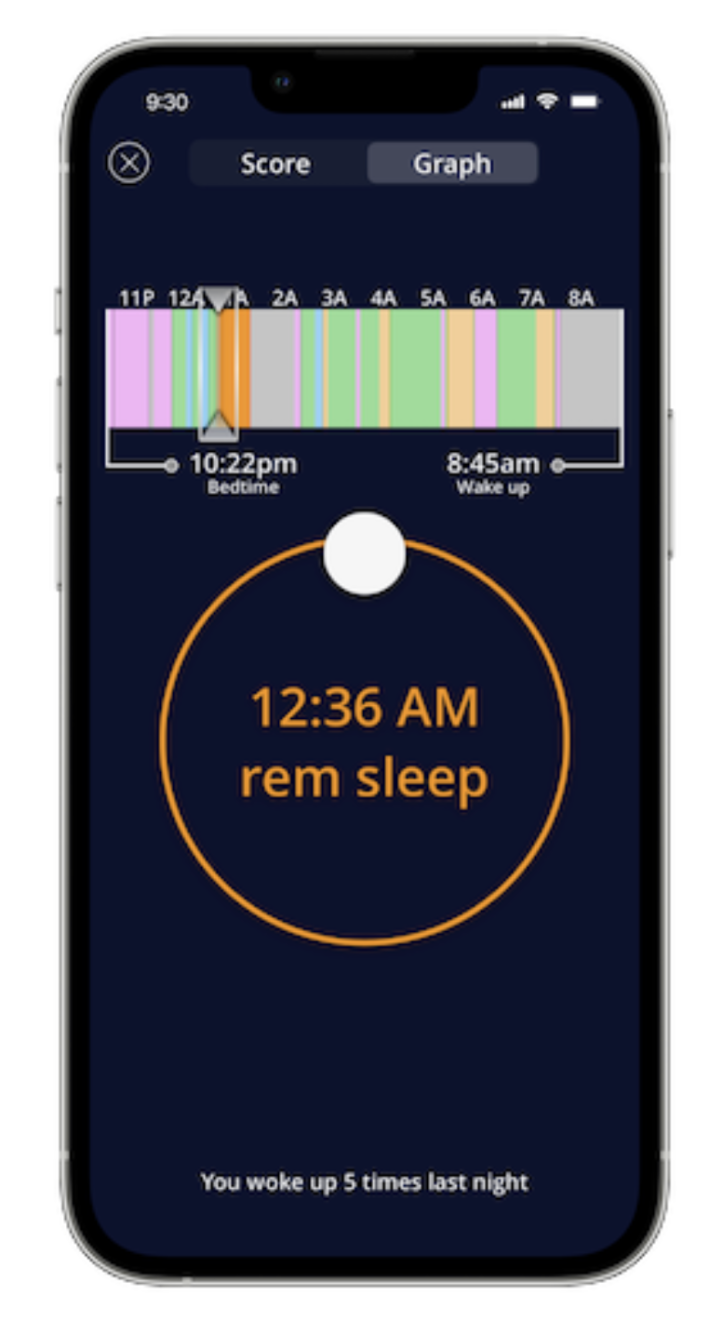
Early Warning Signs in Sleep Patterns
In clinical practice, changes in sleep are often the earliest relapse marker.
Warning signs for mania:
Needing less sleep but not feeling tired
Feeling “wired” at night
Staying up to work on projects
Reduced insight about fatigue
Warning signs for depression:
Sleeping much more than usual
Difficulty getting out of bed
Nighttime rumination
Irregular sleep–wake cycle
Tracking sleep can sometimes be more predictive than tracking mood alone.
What Protecting Sleep Actually Means
Clinically, that often includes:
Fixed wake time (anchor habit)
Avoiding drastic schedule shifts
Limiting late-night stimulation
Cautious use of alcohol
Monitoring travel across time zones
Addressing insomnia early
For some patients, short-term sleep medications may be used strategically. For others, behavioral approaches are sufficient.
References
Harvey, A. G. (2008). Sleep and circadian rhythms in bipolar disorder: seeking synchrony, harmony, and regulation. American Journal of Psychiatry, 165(7), 820–829.
Frank, E., et al. (2005). Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archives of General Psychiatry, 62(9), 996–1004.
Wehr, T. A., et al. (1987). Sleep reduction as a final common pathway in the genesis of mania. American Journal of Psychiatry, 144(2), 201–204.
Leibenluft, E., et al. (1996). Sleep and circadian rhythms in bipolar disorder. Journal of Affective Disorders, 38(2–3), 79–88.
Takaesu, Y. (2018). Circadian rhythm in bipolar disorder: A review of the literature. Psychiatry and Clinical Neurosciences, 72(9), 673–682.
Gold, A. K., et al. (2018). The role of sleep disturbance in bipolar disorder. Current Psychiatry Reports, 20(9), 1–9.
Clinically Reviewed By: